Schedule an Appointment: (770) 771-6991
Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD) is a common and serious vascular condition that can be painful and can create uncomfortable leg symptoms. More than 1 in 20 people in the United States aged 50 and older have peripheral artery disease (PAD). PAD can impact mobility and quality of life. It can also place you at increased risk for stroke, heart attack, and limb amputation.
Early treatment is needed to prevent the progression of PAD. Our specialist is an expert in treating vascular conditions and is dedicated to improving patients’ quality of life. Early intervention is important to producing the best health outcomes. It is important to recognize the early signs and symptoms of peripheral artery disease.
Symptoms of Peripheral Artery Disease
The most common symptom of PAD is claudication. Claudication is muscle pain or weakness that begins with physical activity, such as walking, and usually stops within minutes after resting. Claudication is experienced in about one in four patients.
Other Common PAD signs and symptoms include:
- Difficulty walking or climbing stairs
- Leg pain, cramping, or numbness
- Leg fatigue or heaviness
- Leg discoloration
- Loss of hair on legs
- Foot and leg pain that disturbs sleep
- Shiny skin on the legs
- Non-healing wounds on feet or legs
- One leg that is cooler than the other
- Erectile dysfunction
- Cold or numb toes
- Poor toenail growth
40% of patients have no leg symptoms at all.
Causes and Risk Factors for Peripheral Artery Disease
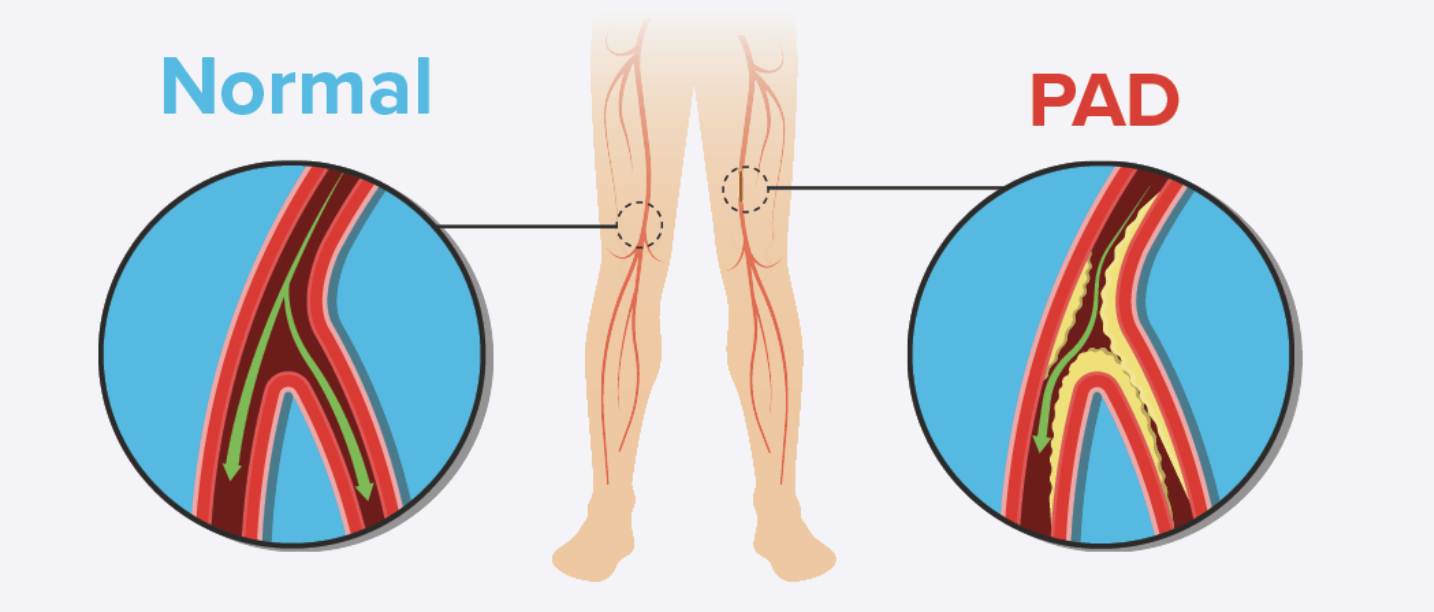
PAD is caused by atherosclerosis, a condition that occurs when plaque builds up in the arteries. Atherosclerosis can lead to a narrowing or blockage of blood flow in the arteries leading to the lower extremities. When sufficient blood and oxygen is unable to reach your legs, a range of painful symptoms can develop. Arteries are responsible for carrying blood and oxygen throughout the body.
Risk factors for PAD:
- Race
- Age
- Sex
- Diabetes
- Smoking
- Poor Diet
- Inactivity
- High cholesterol
- High blood pressure
- Chronic kidney disease
If you have three or more risk factors your increased risk for PAD increases by 10-fold.
Diagnosing Peripheral Artery Disease
If you are at risk for PAD, your doctor may order medical tests to make a diagnosis.
- Ankle-brachial index (ABI): Most commonly, an ABI exam is used to diagnose PAD. This minimally invasive test takes only a few minutes and compares the blood pressure in your ankle with that of your arm.
- Duplex Arterial Ultrasound: A procedure that uses sound waves to create a color map of the arteries in the legs to identify the narrowing of the arterial vessels.
PAD: A Progressive Disease
With peripheral artery disease (PAD) symptoms get worse over time, leading to more serious health conditions. Without treatment, your disease may progress in the following ways:
- Early disease: At this stage individuals are usually unaware that they have PAD. Many people do not experience symptoms. It is possible to have PAD and not be aware of it.
- Moderate disease: You may experience leg pain at rest or develop skin changes like discoloration and non-healing wounds As PAD progresses, claudication can become severe during this stage and impact daily activities. In severe cases, critical limb ischemia (CLI) can develop. CLI occurs when adequate blood supply fails to reach one or more limbs. If left untreated, it can result in limb amputation.
- Advanced disease: At this stage treatment options are limited. Limb amputation may be required due to tissue death and dry gangrene (dry, black skin).
Prevention of Peripheral Artery Disease
Lifestyle changes can help reduce the risk of PAD. Making these simple changes can help:
- Be more physically active
- Eat a healthy, well-rounded diet
- Quit smoking
- Manage underlying health conditions
- Attend routine health screenings
Making these changes can be challenging at times, please enlist the help of a doctor or registered dietician for assistance. Participate in supervised exercise program or join a smoking cessation program.
Chronic peripheral artery disease can impact your quality of life. There is no cure for PAD but it is a treatable condition. Early treatment tends to lead to the best health outcomes. The goals of treating peripheral artery disease early includes alleviating symptoms, reducing health risks, and improving quality of life.
What can happen if PAD is not treated?
PAD places you at increased risk for the following conditions:
- Heart attack
- Stroke
- Limb amputation
Take proactive measures by getting PAD treated to prevent these conditions from happening.
Does Peripheral Artery Disease Affect Other Parts of the Body?
The health of your arteries can impact other parts of the body. While PAD impacts the lower extremities it can also restrict blood flow to your brain and other organs. For men, some may experience erectile dysfunction.
Can Anyone get PAD?
Women and men are affected by PAD. Females are more often asymptomatic than their male counterparts. Women are also more likely to have severe ischemia.
Can I fly with PAD?
Before flying talk to your doctor for recommendations. The prolonged sitting can impact blood circulation. Which may agitate your symptoms.
- Drink plenty of water
- Carry medications on board
- Get up and walk around when possible
- Stretch or massage your legs while seated
Can Peripheral Artery Disease be cured?
Though PAD is not curable, lifestyle changes and medicines can help manage PAD. If that doesn’t help surgery may be necessary. A cardiovascular specialist can help determine the best path forward for each patient.
What Are the Surgical Treatments for PAD?
If lifestyle changes and medication are not enough there are surgical options that can treat PAD.
Angioplasty and Stenting
Peripheral Angioplasty is a minimally invasive procedure which is performed using a catheter which is temporarily inserted to open narrowed arteries of the legs and its branches. Blockages to the arteries of the legs can cause pain and cramps when walking, a condition known as claudication. Stents may be inserted to maintain healthy blood flow which if left untreated may result in gangrene and infection, which may lead to amputation.
Stenting is a procedure in which your cardiologist inserts a slender, metal-mesh tube, called a stent, which expands inside your artery to increase blood flow in areas blocked by plaque. In atherosclerosis or hardening of the arteries, plaque builds up in the walls of your arteries as you age. As more plaque accumulates, your arteries can narrow and stiffen. The stent is a tiny, coiled wire or mesh that is permanently placed at the angioplasty site acting as a scaffold to maintain the new opening.
Atherectomy
The goal of an atherectomy is to remove the buildup of plaque in your arteries. A catheter is used to accomplish the removal. The catheters work in different fashion, they cut and remove the plaque with a sharp rotating blade, vaporization of the plaque, or pulverizing the plaque into micro-particles with high-speed rotating burrs. Under local anesthesia, the catheter is inserted into the artery through a small puncture in the artery, usually in the groin.
Schedule an Appointment
Village Podiatry Centers has multiple locations ready to care for your lower extremity needs.

Village Podiatry Centers provides the highest quality integrated lower extremity care to patients in need through a skilled and compassionate team. We strive to deliver care in a consistent and high-quality manner.
Navigation